Release time :2023-01-06
Source:support@yingchitech.com
Scan:954
Since the 1980s, Transcranial Magnetic Stimulation (TMS) has been used to study the nerve fibers that carry information about movements from the brain to the spinal cord and on to the muscles. In 2004, Chinese Taiwanese scholar Ying-Ju Huang first proposed the theta burst stimulation (TBS) model and proved that it is safe and can target specific populations of neurons in the motor cortex.[1] Subsequently, the clinical use of TBS has become increasingly valuable and plays an important role in the treatment of related diseases.
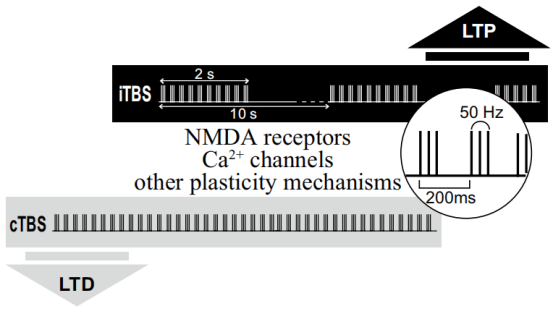
Through all these research over many years, the fnal TBS protocol of rTMS in humans involved the application of three bursts of 50 Hz stimulation, delivered at an interburst interval frequency of 5 Hz and an intensity of 80% AMT. When applied continuously, for a period of 20 or 40 s (300 or 600 pulses), known as ‘continuous’ theta burst stimulation or ‘cTBS’, this led to an LTD-like reduction in MEP size and corticospinal activity lasting for up 20 or 60 min, respectively, after stimulation. Conversely, an intermittent pattern of stimulation (known as ‘intermittent’ theta burst stimulation or ‘iTBS’), in which 600 pulses are delivered in 2 s trains of theta burst stimulation repeated every 10 s for 20 cycles (a total of 190 s), led to signifcant LTP-like increases in MEP size and excitability for up to 20 min.[2][3]
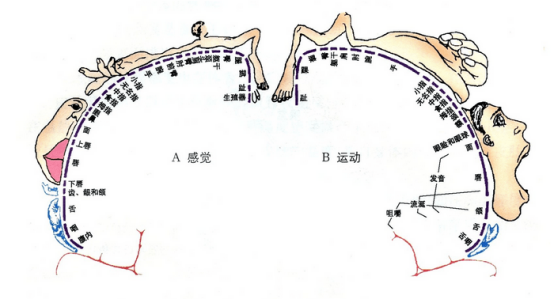
The primary motor cortex directs movement by controlling muscle contractions.In the 1930s, Wilder Penfield and Edwin Boldrey found electrical stimulation of small areas of the frontal lobes sparked movement. The researchers uncovered a map of motor control in this area vaguely corresponding to the layout of the human body. This map-called the homunculus-represents the density of brainpower assigned to controlling different of parts of the body. Those that require fine motor control and have dense nerve stimulation-like the hands and face-are huge, while parts of the body with less-precise motor control, like the legs and torso are much smaller. The primary motor cortex constantly communicates with the basal ganglia, the cerebellum, and areas of the cerebral cortex to ensure movements are intentional, precise, and coordinated with our sensory perception.
Some studies have shown that TBS mode has no significant difference in treatment effect compared with conventional rTMS, but under the same pulse number treatment scheme, it can greatly save the treatment time of a single patient and improve the utilization rate of equipment. [4]And because of its short treatment time, it is suitable for children, cognitive disorders and other patients with poor compliance.
The research team of Chang Gung Memorial Hospital in Taiwan, China published an article that iTBS stimulation combined with virtual reality (VR) upper limb bicycle training was used to restore upper limb motor function after stroke. The result show that the federated method can reduce spasticity, increase actual use of the affected upper limb, and improve participation in daily life in stroke patients.[5]
| target | frequency | intensity | interval | total pulses | Course of treatment |
| M1(affected hemisphere) | iTBS | 80%AMT | 10min | 1200 | 15 |
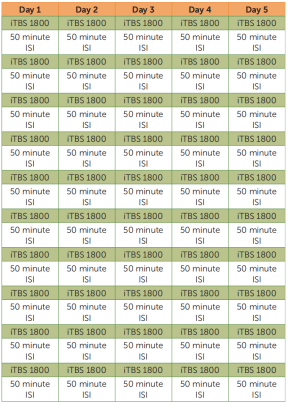
The Stanford Accelerated Intelligent Neuromodulation Therapy (SAINT), a new TBS-based treatment for refractory depression, was recently developed by Stanford University School of Medicine and published in the American Journal of Psychiatry. The protocal is that fifty iTBS sessions (1,800 pulses per session, 50-minute intersession interval) were delivered as 10 daily sessions over 5 consecutive days at 90% resting motor threshold (adjusted for cortical depth).[6] The results of the study found that the Montgomery-Åsberg Depression Rating Scale scores of patients decreased significantly after treatment with no adverse effects. The treatment was found to be significantly effective and safe for the treatment of refractory depression.
[1] Huang YZ, Rothwell JC. The effect of short-duration bursts of high-frequency, low-intensity transcranial magnetic stimulation on the human motor cortex. Clin Neurophysiol. 2004;115(5):1069-1075. doi:10.1016/j.clinph.2003.12.026
[2] Rounis E, Huang YZ. Theta burst stimulation in humans: a need for better understanding effects of brain stimulation in health and disease. Exp Brain Res. 2020;238(7-8):1707-1714. doi:10.1007/s00221-020-05880-1
[3] Huang YZ, Edwards MJ, Rounis E, Bhatia KP, Rothwell JC. Theta burst stimulation of the human motor cortex. Neuron. 2005;45(2):201-206. doi:10.1016/j.neuron.2004.12.033
[4] Blumberger DM, Vila-Rodriguez F, Thorpe KE, et al. Effectiveness of theta burst versus high-frequency repetitive transcranial magnetic stimulation in patients with depression (THREE-D): a randomised non-inferiority trial [published correction appears in Lancet. 2018 Jun 23;391(10139):e24]. Lancet. 2018;391(10131):1683-1692.
[5] Chen YH, Chen CL, Huang YZ, et al. Augmented efficacy of intermittent theta burst stimulation on the virtual reality-based cycling training for upper limb function in patients with stroke: a double-blinded, randomized controlled trial. J Neuroeng Rehabil. 2021;18(1):91. Published 2021 May 31. doi:10.1186/s12984-021-00885-5
[6] Cole EJ, Stimpson KH, Bentzley BS, et al. Stanford Accelerated Intelligent Neuromodulation Therapy for Treatment-Resistant Depression. Am J Psychiatry. 2020;177(8):716-726. doi:10.1176/appi.ajp.2019.19070720