Release time :2022-07-25
Source:support@yingchitech.com
Scan:1037
Obsessive-compulsive disorder (OCD) is a common, chronic, and oftentimes disabling disorder characterized by unwanted and distressing thoughts (obsessions) and repetitive behaviors that the individual feels driven to perform (compulsions).[1]
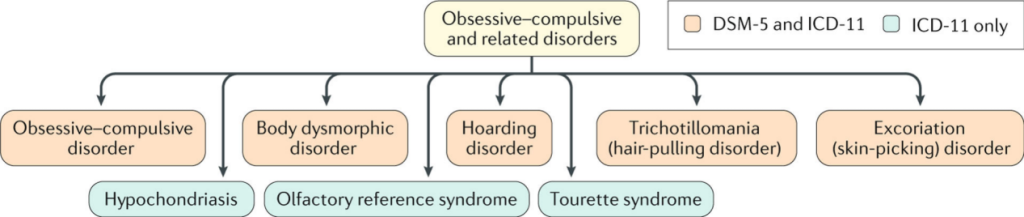
Fig. 1 Obsessive–compulsive and related disorders.
Obsessions are repetitive and persistent thoughts, images, impulses or urges that are intrusive and unwanted, and are commonly associated with anxiety.
Compulsions are repetitive behaviours or mental acts that the individual feels driven to perform in response to an obsession according to rigid rules, or to achieve a sense of ‘completeness’.[2]
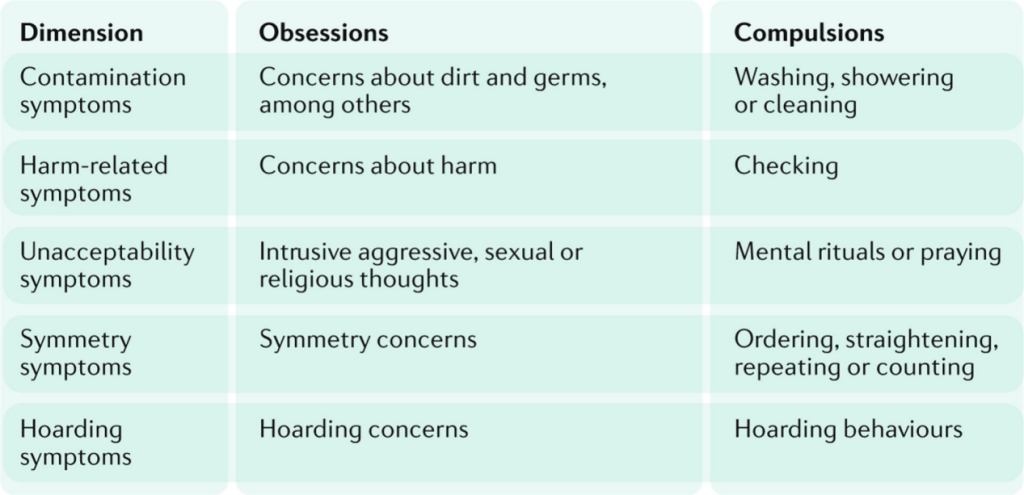
Fig. 2 OCD symptom dimensions.
While these compulsive behaviors are meant to help reduce anxiety, in time they are incorporated into the individual’s obsessive OCD patterns, until they begin inducing stress themselves. This creates a cycle of thoughts and actions that exhaust the individual experiencing them, causing them a great deal of despair.
Prevalence and demographics: OCD was initially believed to be quite rare. However, the first rigorous community surveys that used operational criteria for the diagnosis of mental disorders demonstrated that OCD was one of the most prevalent mental disorders, and OCD was estimated to make a considerable contribution to the global burden of disease. According to the DSM V, OCD occurs in 1.2% of the population. While females are found to be affected at a slightly higher rate than males, males are more likely to develop OCD during childhood.
Risk factors for OCD: OCD has been found to be associated with a number of risk factors, such as genetics, environmental factors, temperament and critical life events. Those with OCD also often battle additional mental health conditions, with three in four having a history of anxiety disorders, and nearly one in two battling depression.
TMS is a non-invasive neuromodulation technology. The time-varying pulsed magnetic field can penetrate the skull non-invasively, act on the central nervous system, generate induced currents, and cause a series of physiological and biochemical reactions, thereby affecting metabolism and neuronal excitability in the brain so that improve and treat mental and neurological diseases.
A randomized crossover pilot study using F8c coil published in 2019 by the Journal of neural transmission confirmed the treatment’s efficacy, concluding that intermittent TBS (iTBS) paradigm over the left dorsolateral prefrontal cortex (L-DLPFC) as add-on treatment significantly improved OCD symptoms.” iTBS is also safe to combine with other forms of therapy, and does not cause any adverse or long-lasting side effects. It is non-invasive and can be easily incorporated into the patient’s daily schedule.[3]
In this paper, TMS OCD treatment using the F8c coil significantly alleviates OCD symptoms.
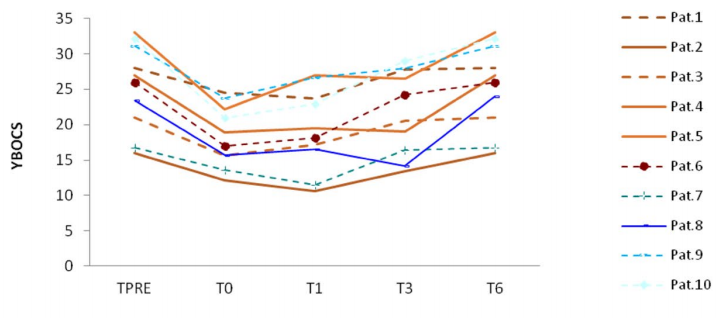
The 2019 study concluded that after one month of treatment, there was a statistically significant improvement in OCD symptoms for the study’s participants when compared to baseline. We found that all the patients improved in OCD symptomatology up to T1, while four among them improved up to T3. These patients were those showing a more extensive reshape of frontal areas phase synchronization and frontoparietal coherence compared to the other participants.
The primary measuring system used in this study was the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS), the gold standard measure of OCD symptom severity. It found that all the patients improved in OCD symptomatology up to T1, while four among them improved up to T3. These patients were those showing a more extensive reshape of frontal areas phase synchronization and frontoparietal coherence compared to the other participants.
As a non-invasive treatment course, none of the patients reported any adverse effect during and after the training in this paper.
TMS has been proven to be a safe treatment option by a number of studies. A 2018 study[4] published by Brain Stimulation Journal highlighted TMS safety, finding it to be a safe OCD treatment: “TMS stimulation over the mPFC (medial prefrontal cortex) and ACC (anterior cingulate cortex) is a safe and effective intervention for improving OCD symptoms in patients who failed to receive sufficient benefit from treatments with SRIs and CBT.”
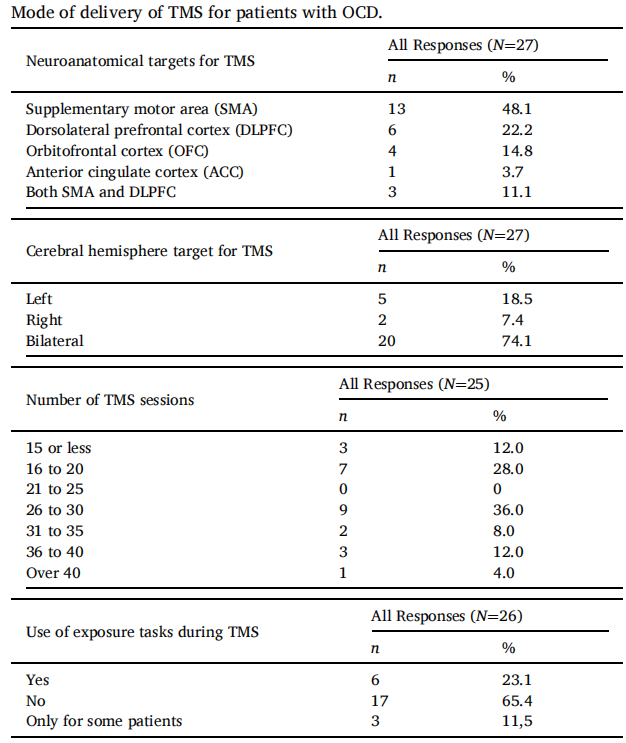
An international survey of different TMS protocols for patients with OCD published in 2021 by Psychiatry Research , aims to evaluate current preferences and trends in the delivery of TMS for OCD. A 10-item online questionnaire was developed and conducted online between April to June 2020, surveying providers of TMS for patients with OCD internationally. A total of 27 valid responses were analysed from 10 countries. The most common target for TMS was the supplementary motor area and stimulation was commonly given bilaterally, but techniques differed between centres. Exposure tasks were not commonly used during TMS. The study calls for more research clarifying the best mode of TMS delivery for OCD.[5]
Reference
[1] American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 5th ed.
Washington, DC, American Psychiatric Association, 2013.
[2] Stein DJ, Costa DLC, Lochner C, et al. Obsessive-compulsive disorder. Nat Rev Dis Primers. 2019;5(1):52. Published 2019 Aug 1. doi:10.1038/s41572-019-0102-3
[3] Naro A, Billeri L, Cannavò A, et al. Theta burst stimulation for the treatment of obsessive-compulsive disorder: a pilot study. J Neural Transm (Vienna). 2019;126(12):1667-1677. doi:10.1007/s00702-019-02098-6
[4] Carmi L, Alyagon U, Barnea-Ygael N, Zohar J, Dar R, Zangen A. Clinical and electrophysiological outcomes of deep TMS over the medial prefrontal and anterior cingulate cortices in OCD patients. Brain Stimul. 2018;11(1):158-165. doi:10.1016/j.brs.2017.09.004
[5] Brakoulias V, Nguyen PHD, Lin D, Pham NDK. An international survey of different transcranial magnetic stimulation (TMS) protocols for patients with obsessive-compulsive disorder (OCD). Psychiatry Res. 2021;298:113765. doi:10.1016/j.psychres.2021.113765